|
Research Article
A prospective comparison of continuous wave and micropulse transscleral laser cyclophotocoagulation for refractory glaucoma in African eyes
1 Consultant Ophthalmologist, Eye Foundation Hospital, 27 Isaac John Street, GRA Ikeja, Lagos, Nigeria
2 Senoir Registrar, Eye Foundation Hospital, 27 Isaac John Street, GRA Ikeja, Lagos, Nigeria
Address correspondence to:
Olufemi Oderinlo
Eye Foundation Hospital, 27 Isaac John Street, GRA Ikeja, Lagos 001001,
Message to Corresponding Author
Article ID: 100008O02OO2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Oderinlo O, Ogunro A, Hassan A, Oladeji A, Idris O. A prospective comparison of continuous wave and micropulse transscleral laser cyclophotocoagulation for refractory glaucoma in African eyes. Edorium J Ophthalmol 2023;6(1):1–6.ABSTRACT
Aims: To report the efficacy of transscleral diode laser photocoagulation and compare outcomes between the continuous wave (CW) and micropulse wave (MP) protocols for refractory glaucoma in African eyes.
Methods: A non-randomized prospective comparative study of patients who had transscleral diode laser photocoagulation for refractory glaucoma between January 2021 and December 2021in Eye Foundation Hospital Lagos, Nigeria was done.
Results: A total of 52 eyes of 52 patients were analyzed. Mean age of patients was 66 ± 12.5 years. The mean preoperative intraocular pressure (IOP) was 31.2 ± 11.9 mmHg. Overall post-operative mean IOP was 17.9 ± 8.6 mmHg at 4 weeks, 21.0 ± 9.9 mmHg at 8 weeks and 20.6 ± 11.4 mmHg at 12 weeks. The difference between mean preoperative and postoperative IOP measured at week 12 was statistically significant (p<0.001). Both continuous wave and micropulse wave protocols were effective at reducing intraocular pressures, the micropulse group had a mean difference between preoperative IOP and postoperative IOP at week 12 of 7.5 ± 6.7 mmHg (p=0.001), while the continuous wave laser group had a mean difference of 11.7 ± 13.7 mmHg (p<0.001). The micropulse group achieved a higher percentage of success in 11 eyes (78.6%) compared with 24 eyes (63.2%) in the continuous wave group. This difference was not statistically significant (p=0.341).
Conclusion: Both the continuous wave (CW) and micropulse wave (MP) protocols of transscleral diode laser photocoagulation were found effective at significantly reducing IOP in our study of African eyes with refractory glaucoma. Although the MP group achieved a higher percentage of absolute success, this was not statistically significant.
Keywords: Continuous wave transscleral laser photocoagulation, Micropulse transscleral laser photocoagulation, Refractory glaucoma, Transscleral laser cyclophotocoagulation
INTRODUCTION
Transscleral laser cyclophotocoagulation (TLC) has shown promising results in the treatment of refractory glaucoma and practically replaced cyclocryotherapy due to better outcomes, efficacy, increased safety, and tolerability [1],[2]. Two protocols of TLC have gained more popularity as effective modalities, TLC with the semiconductor diode laser and TLC with the Nd:YAG laser [3],[4],[5]. Despite several studies evaluating outcomes after TLC there is still no consensus on the ideal dose and laser parameters [6],[7],[8].
Recently transscleral cyclophtotocoagulation using a micropulse (MPTLC) laser has been introduced [9],[10]. This new protocol seeks to improve outcome with fewer side effects. It delivers repetitive short pulses of laser with rest periods in between. These pulses are delivered to the pars plana instead of the pars plicata [9],[10].
This study aims at evaluating the efficacy, safety, and tolerability of two established laser protocols (continuous wave and micropulse) of TLC in a prospective comparison in patients attending a Tertiary Eye Hospital in sub-Saharan Africa.
MATERIALS AND METHODS
A non-randomized prospective comparative study of consecutive patients who had transscleral diode laser photocoagulation for refractory glaucoma between January 2021 and December 2021in Eye Foundation Hospital Lagos, Nigeria was done. Glaucoma was considered refractory when intraocular pressure (IOP) control was not achieved despite maximal tolerated topical and systemic (oral acetazolamide) medications in unoperated eyes, and in painful eyes from terminal glaucoma.
Data were collected using Microsoft excel spreadsheet and data clean-up was done. All records with incomplete data were removed. The cleaned-up data were exported to SPSS ver. 22 for analysis. Quantitative variables such as age, number of medications, IOP, and percentage reduction of IOP from baseline were summarized using mean with standard deviation. Frequencies and percentages were done to summarize categorical variables such as gender, preoperative visual acuities, indications for G-probe laser, the type of G-probe laser, hypotony rate, and success rates. Charts and tables were applied as needed. Paired sample T-test was done to compare mean change in IOP at week 12. Crosstabulation with Pearson Chi-square was used to determine association between outcome measures (success and hypotony rates) and laser types. P value less than 0.05 was considered statistically significant.
Hypotony was defined as postoperative intraocular pressures of less than or equal to 6 mmHg by applanation tonometry. Absolute success was defined as an IOP at 12 weeks or at last visit after treatment of between 6- and 21-mmHg, or an IOP of 22–26 mmHg if pressure reduction of at least 30% compared with pretreatment was achieved, with or without topical medications.
Treatment was conducted under topical (retrobulbar injection of 2.0–4.0 mL of 2% Lignocaine). Using the continuous-wave ARC laser G probe fiberoptic and the ARC micropulse fiberoptic Iris G probe. The ciliary body band location was identified and when not easily visible iris transillumination was used to localize according to the surgeons preference.
The footplate of the G-probe was placed according to the transillumination results and TSC applied 270° of the circumferences either in the supero-temporal or the superior sector, sites of previous surgeries and the 3 and 9 o’clock positions were avoided. The ARC laser maximum output power chosen with the continuous wave probe was 2.5 Watt at 2 seconds per coagulation spot. The average parameter used was 2 Watt at 2 seconds. An average of 20 coagulation spots was applied (on the total circumference maximum 25 spots).
Using the ARC laser micropulse wave probe a special short pulse duration setting of 500 µs pulse duration/1 ms pulse pause was used and 110–130 J was applied with a power setting of 2 Watt. The hand piece was moved continuously over the sclera surface in contrast to the single spot application in the conventional cyclophotocoagulation. The laser was applied all around the eye avoiding the 3 and 9 o’clock positions with a distance of about 1–1.5 mm to the limbus (hand piece edge).
RESULTS
A total of 52 eyes of 52 patients that had adequate records were analyzed, 2 patients with inadequate records were excluded. The mean age of patients was 66 years ± 12.5 years. Ages ranged between 39 years and 87 years. There were 30 males (57.7%) and 22 females (42.3%) giving a male to female ratio of 1.4:1. There were 27 right eyes and 25 left eyes operated.
Advanced Primary Open Angle Glaucoma was responsible for the most common indication for G-probe laser (61.5%). Advanced Angle Closure Glaucoma (AGC) was seen in 1 eye (1.9%), Advanced Primary Open Angle Glaucoma (POAG) in 32 eyes (61.5%), Aphakic/Pseudophakic Glaucoma in 8 eyes (15.4%), Neovascular Glaucoma (NVG) in 10 eyes (19.2%) and Uveitic Glaucoma (UVG) in 1 eye (1.9%). Continuous Wave Transscleral Laser Cyclophotocoagulation (CWTLC) laser was done in majority (38 eyes, 73.1%) while Micropulse Transscleral Laser Cyclophotocoagulation (MPTLC) was performed in 14 eyes (26.9%).
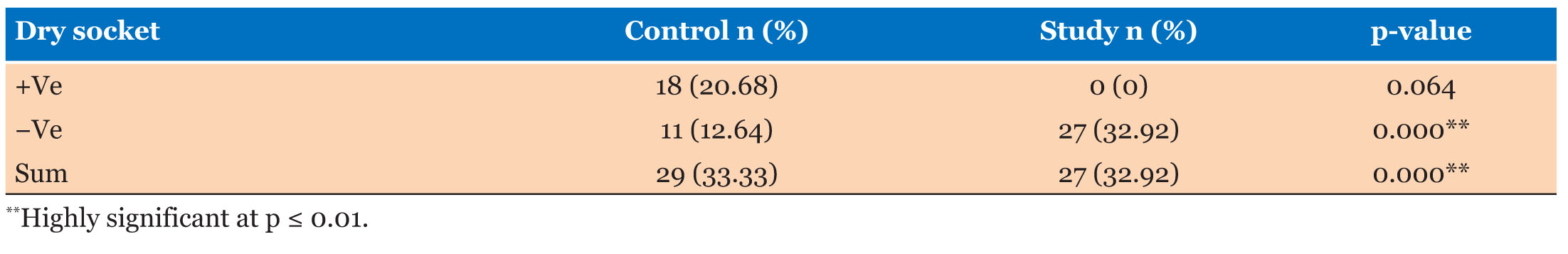
There were no intraoperative complications experienced. Majority did not experience any postoperative complication, (44 eyes, 84.6%), however, 4 eyes (7.6%) had hypotony, 1 eye (1.9%) had a decline in vision, while 2 eyes (3.8%) had hyphema and 1 eye (1.9%) had intraocular pressure spike after the procedure.
Preoperatively, majority (46 eyes, 88.5%) had best corrected visual acuity between NLP to 3/60, the remaining 6 eyes (11.5%) had vision better than 6/60 but less than 6/18, while 45 eyes (86.5%) had best corrected between NLP to 3/60 postoperatively and 7 eyes had vision better than 6/60 but less than 6/18. The mean number of medications being applied preoperatively was 2.4 ± 1.0. Majority (21 eyes, 40.4%) applied 2 medications preoperatively followed by 13 eyes (25%) on 3 medications, while 1 eye (1.9%) was on 1 medication. The overall mean number of IOP lowering medications applied postoperative was 2.7 ± 1.0, 2.7 ± 0.9, and 2.6 ± 0.9 at week 4, week 8, and week 12, respectively. The mean difference in the number of IOP lowering medications at week 12 was -0.2 ± 1.1. This difference was not statistically insignificant (p=0.195).
The mean preoperative IOP was 31.2 ± 11.9 mmHg. At week 4, the mean IOP was 17.9 ± 8.6 mmHg while at week 8 the mean IOP was 21.0 ± 9.9 mmHg. At week 12, the mean IOP was 20.6 ± 11.4 mmHg.
Overall, the mean difference between Preoperative IOP and postoperative IOP at week 12 was 10.6 ± 12.3 mmHg. Using paired sample T test, there was a statistically significant difference between preoperative and postoperative IOP measured at week 12 (t=6.216, 95%CI=7.1–14 mmHg, p<0.001).
The median reduction in IOP from baseline at week 4, 8, and 12 are -46.9 mmHg (IQR -34.3 mmHg), -29.5 mmHg (IQR -37.8 mmHg), and -27.8 mmHg (IQR -43.5 mmHg) respectively.
At week 12, 31 eyes (59.6%) achieved an IOP measurement less than 21 mmHg while 24 eyes (46.2%) achieved more than 30% reduction from baseline.
Thirty-five eyes (67.3%) achieved an absolute success at week 12. Hypotony rate was 7.7% (4 eyes).
Continuous mode laser was responsible for majority (38 eyes, 73.1%) while micropulse G-probe laser was performed in 14 eyes (26.9%). Eleven eyes out of 14 eyes (78.6%) in the micropulse G-probe laser achieved higher absolute success compared with 24 eyes of 38 eyes (63.2%) in the continuous mode G-probe laser, however, this difference was not statistically significant (p=0.341[fishers exact]). The odds of eyes achieving absolute success in the micropulse group over continuous wave was 2.139 (ß=0.760, OR=2.139, p=0.300, CI=0.508–8.998).
In the micropulse group, the mean preoperative IOP was lower than the continuous mode laser group, 22.4 ± 6.9 mmHg vs 34.4 ± 11.8 mmHg respectively.
In the micropulse group the mean difference in IOP between preoperative IOP and postoperative IOP at week 12 was 7.5 ± 6.7 mmHg (t=4.1, 95% CI=3.6–11.4 mmHg, p=0.001) while in the continuous wave mode laser group, the mean difference was 11.7 ± 13.7 mmHg. (t=5.2, 95% CI= 7.2–16.2 mmHg, p<0.001) (Table 1).
Overall, the median visual acuity did not increase following treatment and majority retained preoperative visual acuity. The median preoperative UCVA (decimal) and BCVA were the same 0.0035 (IQR 0.011–0.001). At 4, 8, and 12 weeks the median postoperative UCVA and BCVA remained the same, 0.0035 (IQR 0.011–0.001) respectively. In the continuous mode group, analysis showed that the median preoperative UCVA and BCVA were the same, 0.002 (IQR 0.007–0.001) and at 4, 8, and 12 weeks the median postoperative UCVA and BCVA was not different from the preoperative values, 0.002 (IQR 0.007–0.001) respectively. In the micropulse group, the median preoperative UCVA (decimal) and BCVA (decimal) was 0.005 (IQR 0.013–0.002). At 4, 8, and 12 weeks the median postoperative UCVA and BCVA remained the same, 0.005 (IQR 0.013–0.002) respectively (Table 2).
Rate of hypotony was higher in micropulse G-probe laser group (2 of 14 eyes, 14.3%) compared with continuous mode G-probe laser (2 of 38 eyes, 5.3%). This difference was not statistically significant (p=0.291[fishers exact]).
DISCUSSION
The percentage reduction in IOP postoperatively is one of the major outcome measures used to assess the effectiveness of TLC. In our study, both the continuous wave transscleral cyclophotocoagulation (CWTLC) and the micropulse transscleral cyclophotocoagulation (MPTLC) were effective in reducing the intra ocular pressure in eyes with refractory glaucoma. Overall, the mean difference between preoperative IOP and postoperative IOP at week 12 was 10.6 ± 12.3 mmHg. Using paired sample T test, there was a statistically significant difference between preoperative and postoperative IOP measured at week 12 (t=6.216, 95% CI=7.1–14 mmHg, p<0.001). When the mean difference in IOP was compared to the mean preoperative IOP of 31.2 ± 11.9 mmHg, a 33.9% reduction in IOP was seen 12 weeks post postoperatively. This value is like an approximate 30% reduction in IOP reported from a recent study [11].
Transscleral laser cyclophotocoagulation targets the pigmented epithelium and vascular core of the ciliary body processes to suppress aqueous production. In the CWTLC, tissue photocoagulation is controlled by adjusting the power and duration of exposure. Laser delivered at a continuous dose may result in significant collateral tissue damage and occasionally serious complications, such as uveitis, vision loss, chronic hypotony, and choroidal detachment. The MPTLC is thought to be safer as it delivers a series of repetitive short pulses of energy alternating with rest periods in between pulses. This allows for a “cooling period” with thermal dissipation between bursts, thus potentially minimizing collateral tissue damage [9].
We compared IOP after CWTLC and MPTLC showed, both CW and MP wave protocols were effective at reducing intraocular pressures, the MP group had a mean difference between preoperative IOP and postoperative IOP at week 12 of 7.5 ± 6.7 mmHg (p=0.001), while the CW laser group, had a mean difference of 11.7 ± 13.7 mmHg (p<0.001). However, there was a wider IOP variation in micropulse TLC group represented as wider scattering of points on the scatter plot, (Figure 1) when compared to continuous wave TLC plot in Figure 2.
Postoperative reduction of intraocular pressure is reportedly related to baseline intraocular pressures, with lower baseline pressures resulting in greater improvement [12]. In our study, the micropulse group had lower mean preoperative IOP than the continuous mode laser group (22.4 ± 6.9 mmHg vs 34.4 ± 11.8 mmHg), this likely accounts for the lower difference in postoperative mean IOP when compared to the continuous group.
In further analysis we compared the absolute success of eyes in both groups. The MP group achieved a higher percentage of success in 11 eyes (78.6%) compared with 24 eyes (63.2%) in the CW group. This difference was however not statistically significant (p=0.341). The odds of eyes achieving absolute success in the micropulse group over continuous wave of 2.139 (ß=0.760, OR=2.139, p=0.300 CI=0.508–8.998) was also not significant. This implies that both protocols of treatment are comparable at achieving absolute success in our group of patients.
The safety of any procedure is equally as important as its efficacy, most eyes (84.6%) in our study did not experience any intraoperative or postoperative complication. This is like an overall complication rate of 9% reported by Ansari et al. [13]. Complications reported in this study were hyphema, chronic iritis (>2 months post-treatment), and corneal edema, while those seen in our group of patients were hypotony, a decline in vision, hyphema, and intraocular pressure spike after the procedure. Hypotony is a major concern after TLC, it may result from excessive damage to the ciliary processes causing severe under production of aqueous. The rate of hypotony in our study was overall low, when compared to earlier reports of 39.0% by Ramli et al. [14]. Only 7.6% (4/52) of eyes in our study had hypotony, this was higher in micropulse G-probe laser group (2 of 14 eyes, 14.3%) compared with continuous mode G-probe laser (2 of 38 eyes, 5.3%). This difference was not statistically significant (p=0.291[fishers exact]). There was no significant difference between the number of antiglaucoma medications used before and after surgery, the mean difference in the number of IOP lowering medications at week 12 was -0.2 ± 1.1. This difference was not statistically insignificant (p=0.195). The small number of eyes in our study is a main disadvantage.
A limitation of our study is the large difference between the number of eyes between the two arms of the study, this could decrease the power to detect statistically significant differences.
CONCLUSION
In conclusion both the continuous wave (CW) and micropulse wave (MP) protocols of transscleral diode laser photocoagulation were found effective at significantly reducing IOP in our study of African eyes with refractory glaucoma. Although the MP group achieved a higher percentage of absolute success, this was not statistically significant.
REFERENCES
1.
Assia EI, Hennis HL, Stewart WC, Legler UF, Carlson AN, Apple DJ. A comparison of neodymium: Yttrium aluminum garnet and diode laser transscleral cyclophotocoagulation and cyclocryotherapy. Invest Ophthalmol Vis Sci 1991;32(10):2774–8.
[Pubmed]

2.
Fankhauser F, Kwasniewska S. The role of laser cyclocoagulation in cyclodestructive glaucoma surgery. Curr Opin Ophthalmol 1993;4(2):79–84.
[Pubmed]

3.
Shields MB, Shields SE. Noncontact transscleral Nd:YAG cyclophotocoagulation: A long-term follow-up of 500 patients. Trans Am Ophthalmol Soc 1994;92:271–83.
[Pubmed]

4.
Kosoko O, Gaasterland DE, Pollack IP, Enger CL. Long-term outcome of initial ciliary ablation with contact diode laser transscleral cyclophotocoagulation for severe glaucoma. The Diode Laser Ciliary Ablation Study Group. Ophthalmology 1996;103(8):1294–302. [CrossRef]
[Pubmed]

5.
Brancato R, Carassa RG, Bettin P, Fiori M, Trabucchi G. Contact transscleral cyclophotocoagulation with diode laser in refractory glaucoma. Eur J Ophthalmol 1995;5(1):32–9. [CrossRef]
[Pubmed]

6.
Walland MJ. Diode laser cyclophotocoagulation: Longer term follow up of a standardized treatment protocol. Clin Exp Ophthalmol 2000;28(4):263–7. [CrossRef]
[Pubmed]

7.
Chang SHL, Chen YC, Li CY, Wu SC. Contact diode laser transscleral cyclophotocoagulation for refractory glaucoma: Comparison of two treatment protocols. Can J Ophthalmol 2004;39(5):511–6. [CrossRef]
[Pubmed]

8.
Noureddin BN, Zein W, Haddad C, Ma’luf R, Bashshur Z. Diode laser transcleral cyclophotocoagulation for refractory glaucoma: A 1 year follow-up of patients treated using an aggressive protocol. Eye (Lond) 2006;20(3):329–35. [CrossRef]
[Pubmed]

9.
Aquino MCD, Barton K, Tan AMWT, et al. Micropulse versus continuous wave transscleral diode cyclophotocoagulation in refractory glaucoma: A randomized exploratory study. Clin Exp Ophthalmol 2015;43(1):40–6. [CrossRef]
[Pubmed]

10.
Tan AM, Chockalingam M, Aquino MC, Lim ZIL, See JLS, Chew PT. Micropulse transscleral diode laser cyclophotocoagulation in the treatment of refractory glaucoma. Clin Exp Ophthalmol 2010;38(3):266–72. [CrossRef]
[Pubmed]

11.
Ma A, Yu SWY, Wong JKW. Micropulse laser for the treatment of glaucoma: A literature review. Surv Ophthalmol 2019;64(4):486–97. [CrossRef]
[Pubmed]

12.
Preda MA, Karancsi OL, Munteanu M, Stanca HT. Clinical outcomes of micropulse transscleral cyclophotocoagulation in refractory glaucoma—18 months follow-up. Lasers Med Sci 2020;35(7):1487–91. [CrossRef]
[Pubmed]

13.
Ansari E, Gandhewar J. Long-term efficacy and visual acuity following transscleral diode laser photocoagulation in cases of refractory and non-refractory glaucoma. Eye (Lond) 2007;21(7):936–40. [CrossRef]
[Pubmed]

14.
Ramli N, Htoon HM, Ho CL, Aung T, Perera S. Risk factors for hypotony after transscleral diode cyclophotocoagulation. J Glaucoma 2012;21(3):169–73. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgments
We appreciate Mr. Dipo Odunusil (records staff) for his invaluable contribution to record keeping for our study.
Author ContributionsOlufemi Oderinlo - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Adunola Ogunro - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Adekunle Hassan - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Abiola Oladeji - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Oyekunle Idris - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Olufemi Oderinlo et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.