|
Research Article
Anesthetic effect of lidocaine injection for maxillary teeth with or without tetracaine gel as topical agent during dental extraction in sensitive patients
1 BDS, MSc, Assistant Lecturer, Department of Oral and Maxillofacial Surgery, College of Dentistry, Mosul University, Nenevah, Iraq
2 BDS, FIBMS (MF), Professor, Department of Oral and Maxillofacial Surgery, College of Dentistry, Mosul University, Nenevah, Iraq
Address correspondence to:
Yusra H Al-Mukhtar
BDS, MSc, Assistant Lecturer, Department of Oral and Maxillofacial Surgery, College of Dentistry, Mosul University, Nenevah,
Iraq
Message to Corresponding Author
Article ID: 100046D01YA2024
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Al-Mukhtar YH, Hamid M, Deleme ZH. Anesthetic effect of lidocaine injection for maxillary teeth with or without tetracaine gel as topical agent during dental extraction in sensitive patients. Edorium J Dent 2024;11(2):1–7.ABSTRACT
Aims: Anxiety and fear from dental injections are common and particularly tense features in dental treatment. The direct sense of pain during the injection technique contributes significantly to this dread. The aim of the study was to assess the anesthetic effectiveness and pain of injectable buffered lidocaine with epinephrine with topical tetracaine gel (1%, 1.5%, and 2%) and placebo gel before injection.
Methods: A randomized clinical trial was conducted patients attending the integrated clinics of the dentistry at Mosul University who needed dental surgical treatment. A total of 96 adult patients participated in the study, including 51 males and 45 females. Participants were randomly allocated into four groups, 24 for each one. The injection site was dried with gauze and approximately 0.2 mL of topical anesthetic agent with different concentrations utilized, then after 2 minutes’ local anesthesia, lidocaine with adrenaline with needle gauge 27 was applied for maxillary premolars and molars for infiltration technique and using pain scores as a parameter to assess pain and anxiety sensation. Therefore, the study involves 4 groups. Group A 1%, group B 1.5%, group C 2% tetracaine gel, and group D placebo (ultrasonic gel) as the control group, the data collected and analyzed.
Results: From 96 participants (53.13% male and 46.87% female), there was a highly statistically significant difference between groups regarding pain sensation at time of injection, especially group C with 2% concentration of tetracaine in comparison with other groups.
Conclusion: Topical anesthetics considerably lessened injection and needle insertion pain as compared to the placebo group, also topical anesthesia has a significant psychological impact on patients’ attitudes toward dental treatment, with most patients demanding topical anesthesia before dental injections in order to reduce their level of anxiety and fear toward dental injections.
Keywords: Extraction, Tetracaine, Topical anesthesia
INTRODUCTION
In general, people have a lot of anxiety and fear around dentists and dental procedures. Surveys indicate that 22–79% of people have some degree of dental anxiety [1]. One particularly stressful aspect of dental treatment is injection anxiety. This fear is greatly increased by the immediate feeling of pain experienced throughout the injection procedure [1],[2]. Specifically, topical anesthetics work through pharmacologic and psychological mechanisms to lessen pain and anxiety [3],[4],[5],[6]. Pain may have a greater emotional component than a sensory one in patients with coexisting mental illnesses [4]. To get the best possible pain relief with the fewest possible side effects, pharmacological pain management techniques are a crucial part of pain management plans [5]. In addition, the population with special needs, despite the advances and mobilization for recognizing their demands, has still been facing personal, economic, and social challenges, including difficulties to meet their oral health needs [7]. In the field of health care, disabled patients are mainly assisted by the public healthcare system and higher education institutions. Therefore, both account for collecting, organizing, analyzing, and interpreting data on the current reality, as well as for discussing the services provided by the higher education and health care organizations, including qualification disciplines not available in the undergraduate curricula [8]. In this way, one can observe that undergraduate dental discipline should become adequate and make changes in their curriculum in order to allow professionals to be able to meet the healthcare needs of the population and public [9].
When a local anesthetic is being administered, the pain caused by the needle puncture can be reduced with topical anesthetics [10]. Topical anesthetics have long been widely accepted as a method of reducing needle insertion-related anxiety and discomfort. It is crucial to the atraumatic insertion of local anesthetic [11]. Topical anesthetics can produce surface anesthesia for a depth of 2–3 mm by preventing signals from the sensory neurons’ terminal fibers from conducting. The action-potential threshold rises as a result of this modification, which is secondary to a change in transmission through voltage-sensitive sodium channels. This characteristic of topical anesthesia allows it to successfully reduce the pain associated with needle insertion [12]. The reduction of sodium ion permeability in neuronal membranes by tetracaine limits the start and conduction of nerve impulses, leading to depolarization inhibition, conduction blockage, and ultimately anesthetic action [13]. A number of versions of tetracaine are available, such as an ophthalmic solution for ocular anesthesia, and a gel or solution can be used topically for a localized anesthetic effect. While it takes a short while to start working, perhaps 10–15 minutes, it does so [14]. Since para-aminobenzoic acid is a metabolite of ester-type anesthetics, allergic reactions to tetracaine are conceivable. Ester-type local anesthetics have been shown to cause allergic reactions. A recognized allergy, para-aminobenzoic acid, is released as a metabolite when cholinesterase hydrolyzes ester-type local anesthetics [15]. In our studies, we used tetracaine with different concentrations to evaluate the efficacy of local anesthetics used topically.
Aims of study
This study compares the effectiveness of topical local anesthetic agents with 1%, 1.5%, and 2% tetracaine gel in terms of relieving adult patients’ discomfort during local needle anesthetic administration for upper maxillary infiltration technique.
MATERIALS AND METHODS
A randomized clinical trial studied patients undergoing oral surgery at the integrated clinics in the college of dentistry at Mosul University. In this experimental study, 96 patients were divided into four groups in a blinded fashion. The study was conducted from October 2023 to December 2023. Before starting the study, approval was obtained from the Research Ethics Committee at the College of Dentistry/Mosul University (Ethics approval number UOM. DENT. H.42/22 in 5-1-2023).
Inclusion criteria: Patients over the age of 18 who require local anesthetic along the middle and posterior superior alveolar nerves for maxillary extraction or other dental procedures. And no history of systemic disease or analgesic use prior to joining the clinic.
Exclusion criteria: Patients who smoke were excluded from the study because smoking (salivary albumin and salivary uric acid concentrations are significantly lowered by smoking, and this decrease may be a sign of biochemical changes that may be markers of early periodontal disorders in smokers). Researchers can look into the relationship between smoking-induced diseases and smoking-induced oxidative stress in the oral cavity and periodontal tissues. Dropped levels of salivary albumin and salivary uric acid may be considered markers of the harmful effects of smoking on oral health [16]. Also pregnant or any patient have a history of traumatic local anesthesia administration experiences, or who have sensitivities to the topical anesthetics and patients who did not comply with the protocol of the study excluded from the trial. In addition, participants who could not provide signed consent were barred. Patients with a history of taking analgesics for at least 12 hours before dental surgical treatment were also excluded due to medications like etoricoxib or other nonsteroidal anti-inflammatory drugs (NSAID) such as Naproxen. According to the study by Yusra H. Al-Mukhtar, patients undergoing conventional or surgical tooth extractions may benefit from the preemptive use of etoricoxib to lessen postoperative pain, especially for those taking medication for dental pain relief [17]. A written health history query revealed that all 96 adult patients were in good health in the (18–50 years) age group (51 males, 45 females). The topical anesthesia used in this study is anestocaine manufactured by Sina Darou Tehran, Iran, which is a topical solution for ophthalmic use. Each 100 mL contains tetracaine hydrochloride and benzalkonium chloride as preservatives. Precipitate tetracaine powder and mix it with polyethylene glycol solvent (carboxymethycellulose thickening agent) to manufacture tetracaine gel in three different concentrations (1%, 1.5%, and 2%). Theory Principle: Elastic gel was created by immersing sodium carboxymethylcellulose (CMC) paste in a solution. Carboxymethylcellulose paste was made by combining CMC with polar organic solvent; the solvent replaced the sodium in the carboxymethyl groups with hydrogen (the hydrogen bonds caused the CMC solubility in solution to decrease and formed the elastic gel).
Preparation:
- Gelation (CMC Gel): to 50 mL of vigorously stirring ethylene glycol at 25ºC, gradually add 0.5 gram of CMC (the solute must be added to the solvent to avoid producing a “clump” of solid that is very difficult to dissolve), then continue in the stirring until a clear solution is produced for about 30 min (until the polysaccharide is completely dispersed) to produce a uniform dispersion.
- CMC Gel/Tetracaine (1%): each (11.44 mmol) of CMC gel was added (0.114 mmol) of tetracaine dry powder, then continued in the stirring until a homogenous mixture was produced from a uniform gel.
- CMC Gel/Tetracaine (1.5%): each (11.44 mmol) of CMC gel was added (0.17 mmol) of tetracaine dry powder. Continue in the stirring until a homogenous mixture is produced from a uniform gel.
- CMC Gel/Tetracaine (2%): each (11.44 mmol) of CMC gel was added (0.228 mmol) of tetracaine dry powder. Continue in the stirring until a homogenous mixture is produced from a uniform gel.
The patients were randomly divided into four groups: Group A, given 1% tetracaine gel; group B, 1.5% tetracaine gel; and group C, 2% tetracaine gel. Each group was associated with the control group using ultrasonic gel and regarded as group D, the fourth group. It had placed topical anesthetic gel in the test region and included dipping 0.2 mL of a cotton swab applicator all the way through to coat the affected area. One side of the buccal sulcus had been anesthetized with the study gel, while the other side was covered with the control gel. Then wait for 2 minutes, then the needle was inserted carefully to avoid fear and anxiety-provoking situations in the patients that would alter the pain perception. Visual analog scale (VAS) was given to the patient to record the number of pain perceptions. Patients were instructed that scale 0 represents no pain: VAS = 0, Scale 1 to 3 represents mild pain: 0 < VAS ≤ 3, Scale 2 represents moderate pain; 3 < VAS ≤ 7, and Scale 3: represents severe pain; VAS > 7 [18]. Data were then gathered and analyzed. Patients self-reported their level of pain, and observers recorded their level of discomfort during needle punctured their oral mucosa in order to gauge how well the anesthetic worked. Data analysis was performed using Statistical Package for the Social Sciences (SPSS) version 26 statistical software, taking the relevant variables into consideration. The age and gender were examined using the unpaired t-test, chi-square test, and independent-samples Kruskal–Wallis test. The scores of the groups were compared using the Mann–Whitney U test.
RESULTS
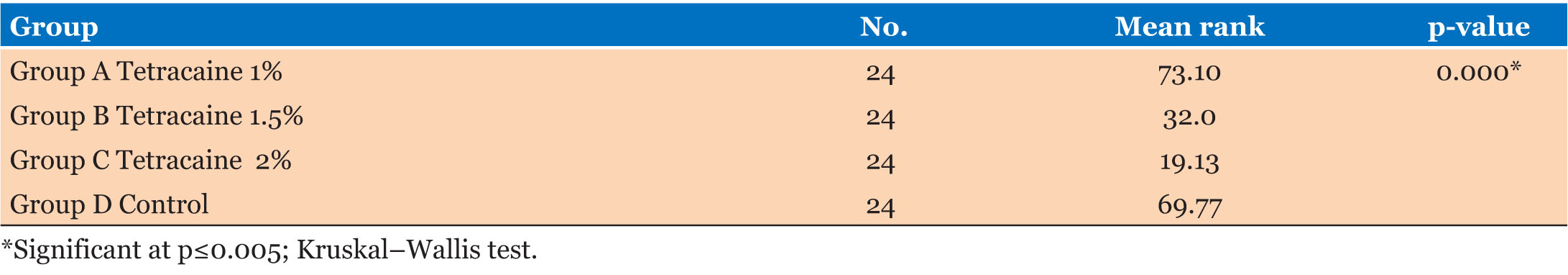
Ninety-six adult (51 males, 45 females) patients participated in the study were in good health and in the age group of 18–50 years. Participants were randomly allocated into four our groups; twenty-four participants in each group. Regarding the pain mean rank score distribution by using a nonparametric test with two independent samples, the Kruskal–Wallis test, the highest was the control group and the lowest was group C tetracaine 2%, which was statistically significant as shown in Table 1.
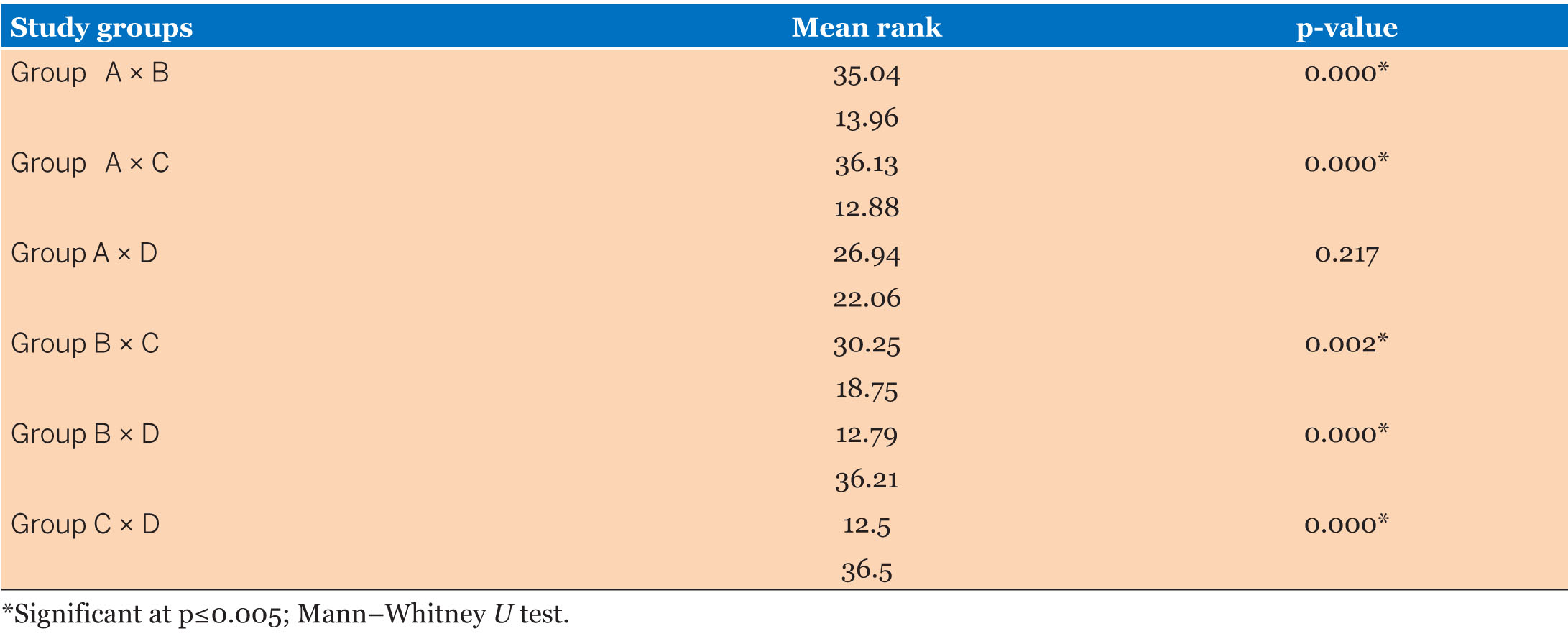
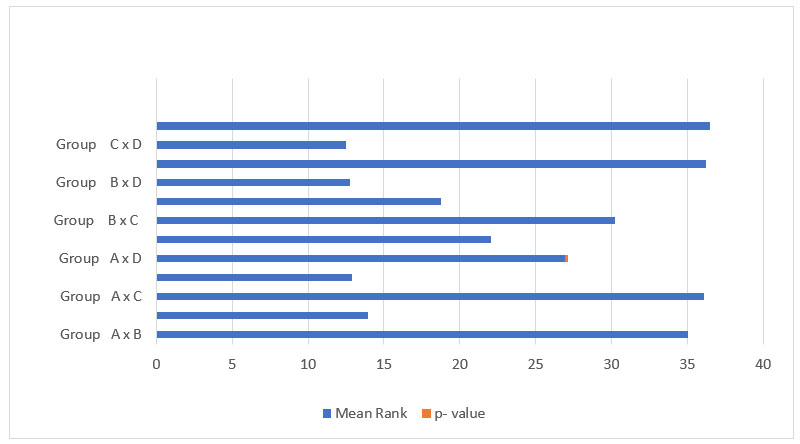
In the comparison of mean pain rank among groups, there was a highly significant difference (0.000) between all groups except groups A and D, which was not significant. That is, the pain score in 1% tetracaine was higher than 1.5% tetracaine concentration, and the lowest pain score was in 2% tetracaine, as shown in Table 2 and Figure 1.
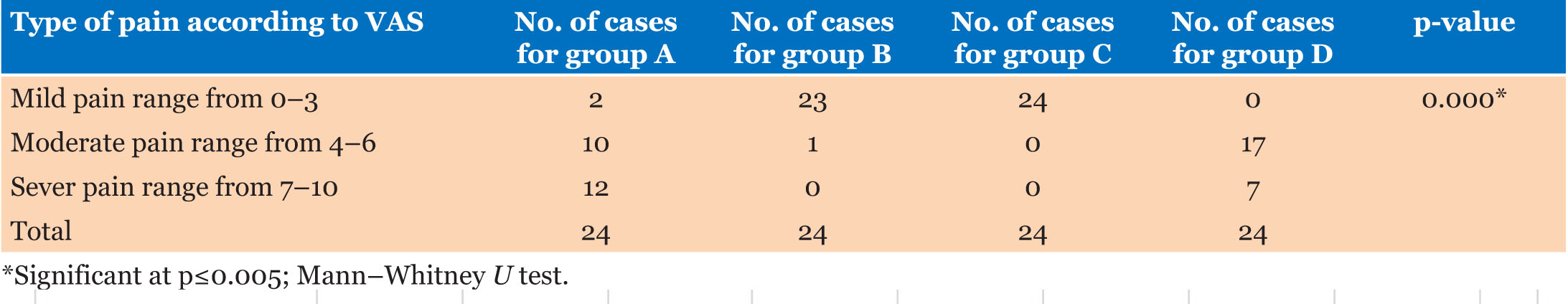
Comparison of type of pain according to VAS among groups, and most participants reported severe pain during the injection for group A, whereas mild pain experienced for groups B and C, and group D was associated with moderate pain. There was a highly significant difference between all groups, as shown in Table 3.
DISCUSSION
The current investigation found that topical anesthesia significantly reduces discomfort during needle penetration and anesthetic solution administration (p≤0.05). To prevent bias related to interindividual differences, the effects of topical anesthetic and placebo treatment were compared in the same individuals’ investigation. Always the patients are distrustful and anxious about dentists as a result of the media’s portrayal of dentistry as an unpleasant discipline, especially when it comes to needle injections. But since most patients see a dentist because they are in pain, and dentists should think about the right pain management techniques to provide the finest pain treatment [19]. In order to induce loss of feeling in the desired body area, local anesthesia blocks the conduction process in peripheral nerves and reduces excitation in nerve endings. In order to slow down the rate of depolarization, local anesthesia operates by decreasing the ion channels’ permeability to sodium [20]. Topical anesthesia has significantly advanced modern dentistry since it may control pain and reduce patient anxiety [21]. The results of several studies examining the efficacy of topical anesthetics were inconsistent [22]. During dental procedures, topical anesthetics are advised to lessen pain, discomfort, and anxiety. But its impact is limited to obstructing the mucosal layer’s superficial layer of discomfort [23]. In a study, Cho et al. assessed the effect of topical anesthetic on needle insertion and injection pain as well as the correlation between patients’ pain scores and anxiety levels. The results showed that topical anesthesia can reduce the pain of both injections and insertions [24]. This result was consistent with our results. Maia et al. study that concluded topical anesthetics can only alleviate pain during needle puncture and in the maxilla [25].
The scientists also reported that the pain from injection was greater than the discomfort from insertion. On the other hand, anxiety sufferers have claimed to experience greater discomfort. Conversely, topical anesthetics have been shown to be effective in reducing anxiety [24],[25].
Topical anesthetics reduce needle stick injury risk and patient anxiety, and last but not least, as previously mentioned by a comprehensive review. Topical anesthetics are an effective and safe technique of pain control, providing a satisfactory level of pain relief when compared to infiltration anesthesia and placebo [26]. All the above research results are consistent with our results in addition to Fatan et al.’s study, the majority of patients request topical anesthetics prior to dental injections in order to lessen their level of worry and panic, demonstrating the substantial psychological impact that topical anesthetics have on patients’ attitudes about dental treatment [27].
Despite some research have found that topical anesthetic is quite helpful in relieving pain during dental treatments; other studies have found conflicting results, showing that topical anesthetic did not significantly reduce pain during injection or needle penetration. The effectiveness of anesthesia was not significantly impacted by injection pain [28]. Other research found no significant influence on the discomfort of needle penetration or anesthetic injection when executing an infiltration injection for maxillary central incisors [29].
CONCLUSION
Topical anesthetics considerably lessened injection and needle insertion pain as compared to the placebo group. Patients with dental anxiety reported less discomfort while using topical anesthetics as opposed to a placebo. Our research demonstrated that topical anesthetics significantly affect patients’ psychological responses to dental care, with the majority of patients requesting topical anesthetics prior to dental injections to lower their level of fear and anxiety related to dental injections. Consequently, we advise concentrating on pain management procedures prior to dental injections.
Future research should aim to improve the efficacy of topical anesthetic by addressing both pharmacologic and psychological variables.
REFERENCES
1.
Khan SD, Alalhareth FA, Moshabab Alyami HF, Ahmed Alnaji MA, Al Touk AA, Saleh Alyami SS. Anxiety among patients undergoing various dental procedures. Bioinformation 2022;18(10):982–5. [CrossRef]
[Pubmed]

2.
Appukuttan DP. Strategies to manage patients with dental anxiety and dental phobia: Literature review. Clin Cosmet Investig Dent 2016;8:35–50. [CrossRef]
[Pubmed]

3.
Mortazavi H, Baharvand M, Far KR, Eznaveh ZS. Dental extraction and full mouth root canal therapy in a patient with atypical odontalgia: Report of invasive malpractice. Braz Dent Sci 2021;24(1):1–4. [CrossRef]

4.
Miura A, Tu TTH, Shinohara Y, et al. Psychiatric comorbidities in patients with atypical odontalgia. J Psychosom Res 2018;104:35–40. [CrossRef]
[Pubmed]

5.
Alorfi NM. Pharmacological methods of pain management: Narrative review of medication used. Int J Gen Med 2023;16:3247–56. [CrossRef]
[Pubmed]

6.
Santos JHL, Gavião MBD, Steiner-Oliveira C, Paschoal MAB, Castilho ARF, Barbosa TS. Translation and cultural adaptation of the Children’s Experiences of Dental Anxiety Measure (CEDAM) to Brazilian Portuguese. Braz Dent Sci 2024;27(1):e4177. [CrossRef]

7.
Anders PL, Davis EL. Oral health of patients with intellectual disabilities: A systematic review. Spec Care Dentist 2010;30(3):110–7. [CrossRef]
[Pubmed]

8.
9.
Ricardo ALF, Yoshida RA, Guaré RO, et al. Dental care for patients with special needs at a private higher education institute. Braz Dent Sci 2023;26(1):e3646. [CrossRef]

10.
Joukhadar N, Lalonde D. How to minimize the pain of local anesthetic injection for wide awake surgery. Plast Reconstr Surg Glob Open 2021;9(8):e3730.
[Pubmed]

11.
Patel D, Lahiri B, El-Patal MAE, Alazmah A, Patel P, Abokhlifa YH. To compare and analyze the potency of two topical anesthetic gels in reducing inferior alveolar injection pain in children of 8–12 years: A double-blinded clinical trial. J Pharm Bioallied Sci 2021;13(Suppl 1):S646–50. [CrossRef]
[Pubmed]

12.
Ship II, Williams AF, Osheroff BJ. Development and clinical investigation of a new oral surface anesthetic for acute and chronic oral lesions. Oral Surg Oral Med Oral Pathol 1960;13:630–6. [CrossRef]
[Pubmed]

13.
Körner J, Albani S, Sudha Bhagavath Eswaran V, Roehl AB, Rossetti G, Lampert A. Sodium channels and local anesthetics-old friends with new perspectives. Front Pharmacol 2022;13:837088. [CrossRef]
[Pubmed]

14.
Almekhyal N, AlOtaibi S, Alenezi Z, Almutairi S, Alharbi F, AlRtam M. Efficacy of tetracaine eye drops in strabismus surgery: A systematic review and meta-analysis of randomized controlled trials. Strabismus 2023;31(3):210–9. [CrossRef]
[Pubmed]

15.
Bina B, Hersh EV, Hilario M, Alvarez K, McLaughlin B. True allergy to amide local anesthetics: A review and case presentation. Anesth Prog 2018;65(2):119–23. [CrossRef]
[Pubmed]

16.
Zarabadipour M, Hosseini SA, Haghdoost-Yazdi H, et al. A study on the correlation between smoking and non-enzymatic antioxidant factors of the saliva of healthy smokers and non-smokers. Braz Dent Sci 2022;25 (1): e2867 [CrossRef]

17.
Al-Mukhtar YH, Deleme ZH, Khudhur AS. Evaluating the efficacy of Etoricoxib in reducing post-operative pain associated with minor oral surgery. A randomized clinical trial. Braz Dent Sci 2023;26(3):e3854 [CrossRef]

18.
Bielewicz J, Daniluk B, Kamieniak P. VAS and NRS, same or different? Are visual analog scale values and numerical rating scale equally viable tools for assessing patients after microdiscectomy? Pain Res Manag 2022;2022:5337483. [CrossRef]
[Pubmed]

19.
Dou L, Vanschaayk MM, Zhang Y, Fu X, Ji P, Yang D. The prevalence of dental anxiety and its association with pain and other variables among adult patients with irreversible pulpitis. BMC Oral Health 2018;18(1):101. [CrossRef]
[Pubmed]

20.
Yang X, Wei X, Mu Y, Li Q, Liu J. A review of the mechanism of the central analgesic effect of lidocaine. Medicine (Baltimore) 2020;99(17):e19898. [CrossRef]
[Pubmed]

21.
Pahade A, Bajaj P, Shirbhate U, John HA. Recent modalities in pain control and local anesthesia in dentistry: A narrative review. Cureus 2023;15(11):e48428. [CrossRef]
[Pubmed]

22.
Park L, Tom J, Bui N, Wilson M, Tanbonliong T. Comparing the efficacy of a compound topical anesthetic versus benzocaine: A pilot study. Anesth Prog 2020;67(1):9–15. [CrossRef]
[Pubmed]

23.
Lee HS. Recent advances in topical anesthesia. J Dent Anesth Pain Med 2016;16(4):237–44. [CrossRef]
[Pubmed]

24.
Cho SY, Kim E, Park SH, Roh BD, Lee CY, Lee SJ, Jung IY. Effect of topical anesthesia on pain from needle insertion and injection and its relationship with anxiety in patients awaiting apical surgery: A randomized double-blind clinical trial. J Endod 2017;43(3):364–9. [CrossRef]
[Pubmed]

25.
Maia FPA, Araujo Lemos CA, de Souza Andrade ES, de Morais SLD, do Egito Vasconcelos BC, Pellizzer EP. Does the use of topical anesthetics reduce the perception of pain during needle puncture and anesthetic infiltration? Systematic review and meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg 2022;51(3):412–25. [CrossRef]
[Pubmed]

26.
Navarro-Rodriguez JM, Suarez-Serrano C, Martin-Valero R, Marcen-Roman Y, de-la-Casa-Almeida M. Effectiveness of topical anesthetics in pain management for dermal injuries: A systematic review. J Clin Med 2021;10(11):2522. [CrossRef]
[Pubmed]

27.
28.
Franz-Montan M, de Paula E, Groppo FC, Silva ALR, Ranali J, Volpato MC. Liposomal delivery system for topical anaesthesia of the palatal mucosa. Br J Oral Maxillofac Surg 2012;50(1):60–4. [CrossRef]
[Pubmed]

29.
Parirokh M, Sadeghi AS, Nakhaee N, Pardakhty A, Abbott PV, Yosefi MH. Effect of topical anesthesia on pain during infiltration injection and success of anesthesia for maxillary central incisors. J Endod 2012;38(12):1553–6. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Yusra H Al-Mukhtar - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mohanned Hamid - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ziad H Deleme - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2024 Yusra H Al-Mukhtar et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.